Do you suffer from back pain that keeps you up at night and makes you feel older than your years?
Chances are, if you are reading this, you are plagued by chronic pain in your back, neck and shoulders that keeps you from doing the activities you enjoy.
Suffering with chronic or acute pain is one of the most frustrating conditions you could possibly experience. You can’t just vacate your body when the pain is too intense, so you wind up missing out on the activities you used to enjoy like cycling, rock climbing, horseback riding, surfing, snowboarding, gardening, and running.
If you’re avoiding activities you love because you’re afraid of making your back pain worse, you’re not alone. Back pain has reached epidemic proportions in America with 4 out of 5 people suffering from disabling back pain during their lifetimes, according to the National Institutes of Health. The American Academy of Orthopedic Surgeons reports that back pain is the second most common reason for doctor’s office visits.
With the medical bill for back pain skyrocketing to a mind-blowing $86 billion dollars a year–up 65% since 1998–we’re not seeing results. The Journal of the American Medical Association reported in 2008 that the percentage of back pain sufferers has increased and more people are reporting physical, social and work limitations as a result.
Sadly, the effects of long-term pain are far more insidious than missed work days and limited mobility. A study conducted by Northwestern University Medical School found that back pain lasting six months or longer results in abnormal brain chemistry, causing the brain to atrophy. Gray matter shrank as much as 11 percent, equivalent to the amount of brain mass that is lost over ten to twenty years of normal aging.
Ongoing back pain runs the risk of clinically impairing your ability to focus and concentrate.
But sadly, although most doctors hear complaints of back pain every single day in their practices,they are ill equipped to fully address the problem.
Standard treatment of back pain in a medical setting generally includes non-steroidal anti-inflammatory medications (NSAIDs), corticosteroid injections such as cortisol, basic physical therapy, and, finally, surgery.
Unfortunately, NSAIDs, such as Aspirin and Ibuprofen, and corticosteroid injections merely mask painful symptoms temporarily.
While medication will give you relief from the feeling of pain, the symptoms will come back when the effects of the drugs wear off because the deeper structural and neurological imbalances that were the root cause of your discomfort were never addressed.
The source of the pain in most cases is not from the spine and surrounding nerves but rather from the muscles, tendons and ligaments that support the anatomy, says Hubert L. Rosomoff, director of the Comprehensive Pain and Rehabilitation Center at the University of Miami School of Medicine.
Even worse, while under the influence of pain relieving medications, you’re likely to be extra active because you’ll feel more like your old self. This brings on additional pain and stiffness later due to the extra stress placed on the already imbalanced soft tissue.
Prescribing pain relieving drugs to treat the symptoms of back pain is like patching a crack in the wall of a house. Sure, the crack is gone, but the underlying instability in the house’s foundation that caused the crack to develop in the first place is still there, and that crack will appear again, if not in the same wall, elsewhere in the home.
As pain progresses and worsens, doctors often turn to surgery as a solution; however, recent studies have shown a failed back surgery rate as high as 50%.
Dr. Alok Sharan, spinal chief at New York’s Montefiore Medical Center, requires that his patients exhaust all non-surgical options prior to an operation. “Sometimes people jump to [back surgery] and think it will be a cure-all, and then five years later you need another procedure. If you’re only 40, that’s a big deal,” he says.
Long term relief can be yours, however, if you understand the basic key to healing back pain. But before we dive into that, I want to share with you some of the commonly held back pain myths that might be responsible for keeping you stuck in pain.
Back Pain Myths That Keep You From Healing
#1 The pain is in your back
This is probably THE most common mistake that people make when treating back pain: looking only at the back. I have seen clients who come in with detailed medical reports that have pinpointed the dysfunctional spinal vertebra seemingly causing all of their problems, and yet repeated treatments in this area are not yielding results.
Your spine does not exist in isolation inside your body. It is a structure who’s balance depends on the balance of everything around it, much like a suspension bridge. Never, not even once, have I worked with someone who suffered from back pain where the problem was entirely in their back. In fact, in 95% of my clients’ cases, the back is the last place we work, and at that point it is only to balance and integrate work done elsewhere.
Looking back at our example of the house with the faulty foundation, your feet, legs, and hips are the “foundation” for your back. If you have an imbalance anywhere in these structures, your back will reflect that. To get lasting relief from back pain, you must build a solid foundation.
#2 Back pain is a sudden-onset condition
It’s very common to assume that your back pain came on in a relatively short period of time. Usually, people notice acute pain after a specific event, like moving heavy furniture or a particularly grueling hike, so it’s easy to associate the pain with these activities.
In reality, the pain is just your body reaching its threshold for the physical imbalances you’ve had all your life. The activity is just a catalyst, the straw that broke the camel’s back, so to speak.
You have certain neurological habits–everyone does. Your coordination was developed at a young age and through repeated training. Sometimes these patterns serve you, and sometimes they hinder you or create muscular imbalances.
Wherever you go, your body will always fire the strongest and most often-used neurological pathways because this is the most efficient way to move. It would really be a chore if you had to relearn to walk every day when you got out of bed! As you get older, your favorite pathways become stronger and stronger, which serves you in efficiency but sets you up for physical pain if they’re not 100% balanced.
To fully address your pain, you must find balanced movement patterns that won’t pull your body more to one side or the other.
#3 Your skeletal alignment (or mis-alignment) is the cause of your pain
This is a half truth. In reality, if your bones are lined up, life is pretty good in your body. Where we get confused is in thinking it’s the bones that determine our body alignment.
Think back to the skeleton that lurked in the corner of your high school science classroom. Did you get to go play with it during anatomy lessons? If you did, you probably noticed that all the bones were wired together and the whole thing hung from a hook.
If you stack up a pile of bones, it won’t stay stacked up. They’ll just fall right down again. It’s the muscles, tendons, and ligaments that keep your bones in place. Bones are really just spacers for your tissue, levers that your muscles can pull on for locomotion.
Your posture is determined by tissue length, not bony alignment. To make lasting changes to your physical alignment, you’ll get much more bang for your buck if you work with soft tissue.
#4 Stretching will take the pain away
Stretching certainly does give good kinesthetic feedback, but I stretched diligently for years and never got one iota more flexible. Why is this?
Well, your muscles are actually plenty long enough. It’s not your muscle’s physical length that inhibits flexibility, but rather the neurological “set point” that keeps you from over stretching it.
For example, imagine an 85 year old man who is so stiff he can barely limp up a flight of stairs. He goes in for surgery and the nurses put him under anesthesia. While under the influence of the drug, the medical staff has to be extremely careful when they move the man because he is so flexible that they can risk dislocating one of his joints. If they wanted to, they could easily tuck his foot behind his head. As soon as the man wakes up and the effects of the anesthesia wear off, however, he is just as stiff as before he went under the drug.
So, if our muscles are long enough to give us all the flexibility we need, why is it so uncomfortable to stretch? The nervous system is responsible for your range of motion. When you “stretch” the muscle, tiny little sensory receptor cells in the tissue send a signal to your brain that you’re getting close to your flexibility threshold beyond which your body believes that your muscle might actually tear. The muscle then contracts in response to prevent over-stretching, and this is the slightly painful feeling you get when you stretch to your full range of motion.
If you incurred an injury, you may have scar tissue that is too fibrous to stretch. If your body is imbalanced–which, if you’re experiencing back pain, it most definitely is–tight muscles are usually compensating for something that’s too loose elsewhere. Thus, pulling endlessly on these muscles trying to get them to lengthen out won’t ever succeed. You have to address both issues.
Additionally, if you haven’t moved a body part for a long time–say you injured your shoulder playing tennis and have favored it ever since–your body will create adhesions in the connective tissue network that prevent your muscles from moving as freely as they once did. It’s imperative to break up these adhesions in order to restore your range of motion.
The True Causes of Back Pain
Back pain is caused by one of two issues in the body: a lack of stability or a lack of mobility. These are actually two sides of the same coin. Where your body is not properly supported–a lack of stability–there will be additional tension to compensate, creating a lack of mobility. Also, if an area of your body is hyper mobile, your muscles will tighten elsewhere to increase the level of support.
In order for your body to function optimally, you must have adequate support. Your body is an incredible feat of engineering, a system of levers and pulleys more complex than any machine we could ever hope to create. Each tiny joint in your body supports a system of joints above and below it. Irregularities in movement in one tiny area of the body can affect the functioning of everything else.
If we look at a body in standing, we can see that the foot and ankle support the knee, which in turn supports the hip joint. Misalignments in any of these three will cause the pelvis to be uneven.
The sacrum–a large, triangular bone at the base of your spine comprised of fused vertebra–fits into the pelvis much like the keystone of an arch. If the two pelvic bones are imbalanced, it will torque the sacrum, putting strain on the sacro-illiac joints and causing lower back pain.
An imbalanced pelvis also affects the upper back, neck, and shoulders. The sacrum is the foundation of the spine; if it’s rotated or crooked, it will affect all of the vertebra above it. Without a stable base, your upper body will brace to support an upright posture, leaving you with limited range of motion in your neck and shoulders.
Therefore, a misalignment or lack of mobility in your ankle can–and does–affect the functioning of your neck. If you’ve been receiving localized treatment to your spine without results, it’s most likely because the root of the problem lies elsewhere in your body.
It is only through treating the body as a whole, synergistic organism that we can deeply address the structural imbalances that are the root cause of back, neck and shoulder pain.
A Natural Pain Solution
In the 1970s, biochemist Ida P. Rolf pioneered the field of myofascial organization. Continually seeking solutions to her own health challenges and those of her two sons, she explored the fields of homeopathy, osteopathy and chiropractic. As she pursued her research, Rolf discovered a correlation between physical alignment and health, noting that when the body was properly aligned in gravity, symptoms such as pain, inflexibility, anxiety and stress vanished.
Her work, which she called Structural Integration and later came to be known affectionately as “Rolfing,” has been used successfully to treat athletes and active individuals looking to get relief from pain and improve athletic performance for the last 40 years.
Rolfing affects physical alignment through gentle manipulation of the connective tissue matrix. Connective tissue, or fascia, is exactly what it sounds like: tissue that functions as a giant web in your body and covers every bone, nerve, organ, muscle, tendon, and ligament, right down to the cellular level. Adjusting the length of fascia within the body shifts posture by changing the way bones are linked together.
Bones act only as levers and spacers in the body. They give the soft tissue–muscles, tendons and ligaments–something to grab onto in order to generate locomotion and make your body move. So, if the tissue is too tight or too loose, it will actually pull your skeletal structure out of alignment. Fortunately, fascia is rich in tiny receptor cells called proprioceptors, which tell the body where it is in relation to the space around it. By gently stimulating these incredibly smart neurological cells, Rolfers can affect changes in the tissue length and quality, influencing flexibility and range of motion practically instantaneously. That coupled with client awareness and neurological re-education forms the foundation for correcting structural imbalances.
http://www.sxc.hu/profile/igowerf
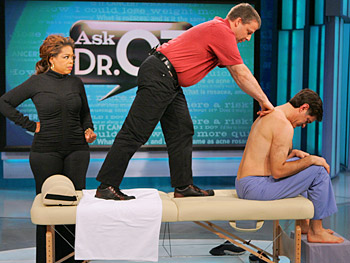
Dr. Oz recommends Rolfing for chronic muscular pain and tension.
“Rolfing literally releases the joints. When you talk to folks about the impact it has on them, a lot of them just stand taller. A lot is just freeing you up to live the way you’re supposed to live.”
– Dr. Oz